Heel Pain, Plantar Fasciitis
Heel pain can be caused by a number of things. However, I will discuss the most common causes of heel pain here. Without doubt the most common cause of heel pain I see as a podiatrist is plantar fasciitis. I will discuss plantar fasciitis later. For now, let’s start with some other causes of heel pain which I will only briefly touch upon.
As with many fractures trauma is often the cause, but what makes one more prone to fractures? Bone can be osteopenic. For example, if a person had a knee surgery and they were in a cast for awhile and the bone becomes weak from disuse, then one maybe more prone to fractures. Long term steroid use, calcium deficiency, older age, and post menopausal women maybe more prone to fractures.
Calcaneal stress fractures maybe a cause of heel pain. It is important to differentiate calcaneal stress fractures from plantar fasciitis as they can often present with similar symptoms. A podiatrist might do what is known as a heel squeeze test by manually compressing both sides of the heel with the palms, and if this is painful then the diagnosis is less likely plantar fasciitis. Imaging is always important, but being cost effective can be tricky. X-rays aren’t very useful in the early stages of a calcaneal stress fracture as it may take 3-4 weeks to show signs on the x-ray. MRI, bone scan, and CT scans are more useful in diagnosis, but then again, it’s not really worth it especially if it isn’t going to change the treatment plan. Now if the pain continues for months with no improvement then advanced imaging such as an MRI or CT scan would be warranted.
One important cause of heel pain I’d like to mention is with children. Heel pain in children, particularly active children/adolescents, is Sever’s Disease, also known as calcaneal apophysitis. This is an inflammation of the growth plate in the heel of children. The symptoms include pain in the heel caused by repetitive stress to the heel. Someone who doesn’t know how to read x-rays well might confuse the inflamed growth plate as a heel fracture. This disease usually resolves once the bone has completed growth or activity is decreased.
Another cause of heel pain is a Haglund’s deformity. This is a bit easier to diagnose as a patient often presents with pain, redness, and swelling along with a “bump” to the posterior-lateral heel. Shoegear often aggravates this condition as it rubs along the area of pain. A patient may also develop hyperkeratosis (corn/callus) or even ulceration at the bump site. Haglund’s deformity is typically seen on x-ray on the lateral view as a podiatrist can see the bump and even use certain measurements (ex: Fowler-Phillip angle). I’m also going to lump Achilles tendonitis into this category as it often presents with similar symptoms but maybe distinguished with an MRI or ruled out with an x-ray. Conservative measures include a heel lift, open back shoes, padding, ice, NSAIDS may help alleviate the pain. Surgical resection in the operating room is the more definitive treatment for Haglund’s deformity.
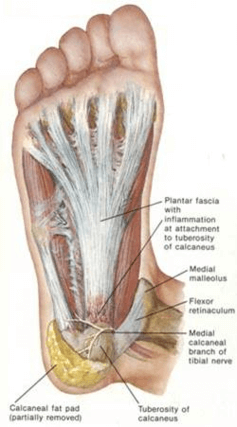
And finally, plantar fasciitis also known as heel spur syndrome. This is reported to be the most common cause of inferior heel pain in adults. In the United States, more than 2 million people are treated for plantar fascitis on an annual basis. It accounts for ~10% of runner-related injuries and ~11-15% of all foot symptoms requiring professional care. So what is the plantar fascia? It is a long, thick band (fascia) that extends from the medial tubercle of the calcaneus and fans out over the bottom of the foot to the metatarsal heads. It is important in forming the longitudinal arch of the foot and functions as a shock absorber. Think of the plantar fascia as a giant rubber band or latex glove connecting at the heel and stretching out to the forefoot. Excessive loading of this fascia can lead to plantar fasciitis.

Call Today to Schedule an Appointment
702 - 518 - 1862There are many risk factors for plantar fasciitis that maybe divided into anatomical, biomechanical, and environmental risk factors. Anatomical risk factors include pes planus, pes cavus, tarsal coalition, obesity, limb length discrepancy, fat pad atrophy, and shortened Achilles tendon. Biomechanical risk factors include equinus, weak plantar flexor muscles or intrinsic muscles of the foot, excessive subtalar joint pronation, poor foot wear, and limited ankle dorsiflexion. Environmental risk factors include trauma, deconditioning, hard surfaces, walking barefoot, prolonged weight-bearing, and inadequate stretching.
Obtaining a history from the patient is very important in diagnosing plantar fasciitis. Typically a patient will report pain on the inferior heel and maybe the arch of the foot as well. The pain is often worse with the first few steps taken in the morning, or if the patient has been inactive and sitting and then suddenly stands to walk. The podiatrist will palpate the patient’s foot and they will often have tenderness at the antero-medial aspect of the heel. Ankle dorsiflexion may be limited due to tightness of the Achilles tendon and pain maybe exacerbated by passive dorsiflexion of the toes.
Diagnosis is usually made from the history and physical examination. Imaging is often used to rule out other causes of the pain. As mentioned, plain radiographs are used to rule out calcaneal stress fractures and other rare bony lesions. On x-ray the patient will often have a heel spur. This heel spur is not actually the source of the pain but is more of a sign of plantar fasciitis as the fascia pulls at this area. Simply removing the spur is not a cure for plantar fasciitis as it is not addressing the primary issue. An MRI maybe used to visualize the plantar fascia particularly with the sagittal and coronal views.
There are many conservative treatments to plantar fasciitis that I discuss here. Treatments include rest, ice, avoidance of aggravating activity, proper shoes (shoes should be changed every 300-500 miles), arch supports and orthotics, avoid going barefoot, arch taping, stretching, physical therapy, NSAIDS, walking boot (severe cases) and night splints. Night splints are used to allow for prolonged passive stretching to allow the fascia to heal, however one may find it difficult to sleep with the night splint on. If the pain is severe a corticosteroid injection is often given into the heel, but it is important to limit these injections as overuse can lead to plantar fascia weakness and rupture.
Surgery is always reserved as a last resort. The most common procedure is a partial plantar fasciotomy. The procedure maybe open requiring a 3-6cm plantar medial incision, or closed utilizing endoscopy to release the fascia. Topaz procedure is also another option. Again, most patients see fantastic results with conservative therapy. It is important to find a good podiatrist who can treat you at the start of your symptoms.
As a 24/7 house & hotel Las Vegas Podiatrist I take pride in my thorough evaluation and treatment of plantar fasciitis and heel pain. Like my ingrown toenail treatment, my treatment of heel pain are backed by peer reviewed journals and research and in my opinion are the best treatment of heel pain and plantar fasciitis. I do not use “cheap” supplies and my inventory is stocked with only the most up to date and high quality supplies. Please call now if you are around Las Vegas and suffer from heel pain, plantar fasciitis, neuroma, ingrown toenail, painful nails, warts, thick and long fungal nails, diabetic feet, or an ankle sprain.
As a 24/7 house & hotel Las Vegas Podiatrist I take pride in my thorough evaluation and treatment of toe pain and ingrown toenails. My treatment of ingrown toenails are backed by peer reviewed journals and research and in my opinion are the best treatment of ingrown toenails. I do not use “cheap” supplies and my inventory is stocked with only the most up to date and high quality supplies.
Please call now if you are around Las Vegas and suffer from heel pain, plantar fasciitis, neuroma, ingrown toenail , painful nails , warts, thick and long fungal nails, diabetic feet , or an ankle sprain. For information on what/why I use for my chemical matrixectomies for ingrown nails please visit this link.
SCHEDULE YOUR CONSULTATION
